NU PICC SimulatorA medical training device to help nurses place PICC lines in neonates
Through a Design Thinking and Communication (DTC) course, a Segal Design Institute Summer Internship and a biomedical engineering capstone project, mechanical engineering major Andrew SaLoutos leads the development of a medical training device that captures widespread interest from practitioners.
Problem
While the traditional healthcare teaching method – see one, do one, teach one – holds value in many instances, it fails as a plausible training practice for inserting PICC lines into neonatal patients. Neonatologists from Chicago’s Lurie Children’s Hospital challenged students to create a reusable, low-cost simulator.
While the developments felt promising all along, the conference confirmed we’re on the right path.Andrew SaLoutos, Team member
Solution
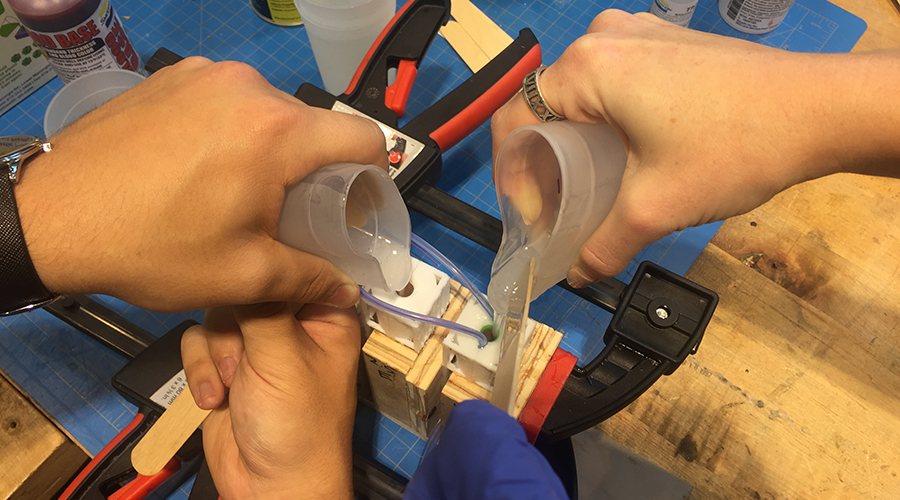 Through a combination of 3-D printing and silicone castings, SaLoutos spearheaded the development of a life-like doll with realistic tissue properties and vasculature geometry as well as pressurized veins.
Through a combination of 3-D printing and silicone castings, SaLoutos spearheaded the development of a life-like doll with realistic tissue properties and vasculature geometry as well as pressurized veins.
Users can prick the doll’s arms or legs, witness “flashback” and then thread a PICC line into the body.
Development Process
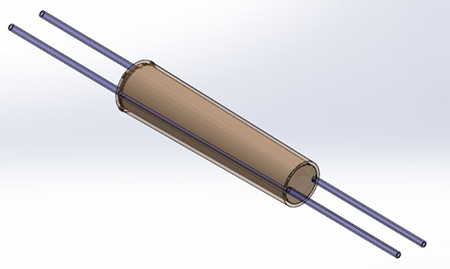 In the fall of 2014, SaLoutos and three freshmen DTC classmates presented Lurie stakeholders their initial solution: a twist-and-lock mechanism that featured arms attached to a torso and two catheter pathways.
In the fall of 2014, SaLoutos and three freshmen DTC classmates presented Lurie stakeholders their initial solution: a twist-and-lock mechanism that featured arms attached to a torso and two catheter pathways.
More than one year later, at the request of Lurie neonatologist Dr. Ann Downey, David Gatchell (director of Segal's MaDE program) contacted SaLoutos to further develop the promising solution.
First through a Segal Summer Internship in 2016 and then during a two-quarter biomedical engineering (BME) capstone course alongside seniors Madisen Rosztoczy, Nataliya Rokhmanova, Kaley Wendorf and Camille Calvin, SaLoutos and his colleagues further tested materials, vein depths, and vein/tissue architectures while also integrating a blood flashback capability.

In February 2017, with support from the biomedical engineering program, Segal’s Norman Design Fund and Northwestern’s Office of Undergraduate Research, Rosztoczy and Rokhmanova attended NEO, the nation’s premier neonatology conference, to exhibit the team’s working prototype.
Attendees praised the product’s realistic attributes and expressed overwhelming interest in its potential as a viable training tool.
“While the developments felt promising all along, the conference confirmed we’re on the right path,” SaLoutos says.
Current Status
The BME capstone team continues it works as part of the Tinker Program at The Garage, Northwestern’s student entrepreneurship hub, where they hope to improve the product’s superficial veins, add more vascular branching in the torso and continue testing.

In time, SaLoutos hopes to publish a paper with Gatchell, Dr. Downey and his BME teammates and work with Northwestern’s Innovation and New Ventures Office to secure a patent.
“The enthusiasm is there with our client and the biomedical engineering program to keep going,” SaLoutos says.
ProgramsDesign Thinking and Communication (DTC)
Faculty AdvisersDavid Gatchell
